When you have a cough, a runny nose, or a sore throat, your first instinct might be to visit a doctor for antibiotics. After all, antibiotics are often seen as a quick fix for many ailments. But here’s the truth: antibiotics are not a cure-all, and using them unnecessarily can do more harm than good.
The World Health Organization (WHO) recently took to Instagram to remind the public of a critical fact: antibiotics do not treat viral infections like colds and flu. This message is part of a broader effort to promote responsible antibiotic use and combat the rising threat of antibiotic resistance.
Antibiotics are powerful medicines designed to treat bacterial infections. They have saved countless lives by effectively combating diseases like pneumonia, tuberculosis, and urinary tract infections. However, their effectiveness is limited to bacterial infections and does not extend to illnesses caused by viruses.
The common cold, Influenza, and most sore throats are viral infections. Taking antibiotics for these conditions not only fails to cure them but also exposes you to unnecessary risks, including side effects and antibiotic resistance.
What Is Antibiotic Resistance?
Antibiotic resistance is a global health crisis. It occurs when bacteria adapt and become immune to the effects of antibiotics, rendering these medications ineffective. According to the Food and Drug Administration (FDA), misusing antibiotics such as taking them for viral infections or not completing prescribed courses contributes significantly to this problem.
Antibiotic-resistant infections are harder to treat, require stronger medications, and often lead to longer hospital stays and higher medical costs. In severe cases, they can even result in death.
Using antibiotics when they’re not needed can lead to a range of problems, including:
1. Common Side Effects: These may include nausea, vomiting, diarrhea, abdominal pain, and skin rashes.
2. Severe Allergic Reactions: For some people, antibiotics can cause life-threatening allergic responses.
3. Increased Risk of Resistant Infections: Misuse can pave the way for bacteria to become resistant, making future infections more challenging to treat.
How to Support Your Body During Viral Infections?
When you’re dealing with a cold, flu, or similar viral illness, it’s essential to focus on supporting your immune system. Here are some practical steps to help your body recover:
1. Rest: Adequate sleep allows your body to focus on healing.
2. Stay Hydrated: Drink plenty of water, herbal teas, and clear broths to keep your body hydrated.
3. Eat Nutrient-Rich Foods: A diet rich in fruits, vegetables, lean proteins, and whole grains can boost your immune function.
4. Manage Symptoms: Use over-the-counter medications like decongestants and pain relievers to ease symptoms, but always follow the instructions.
5. Practice Good Hygiene: Wash your hands regularly, cover your mouth when coughing, and avoid close contact with others to prevent the spread of infection.
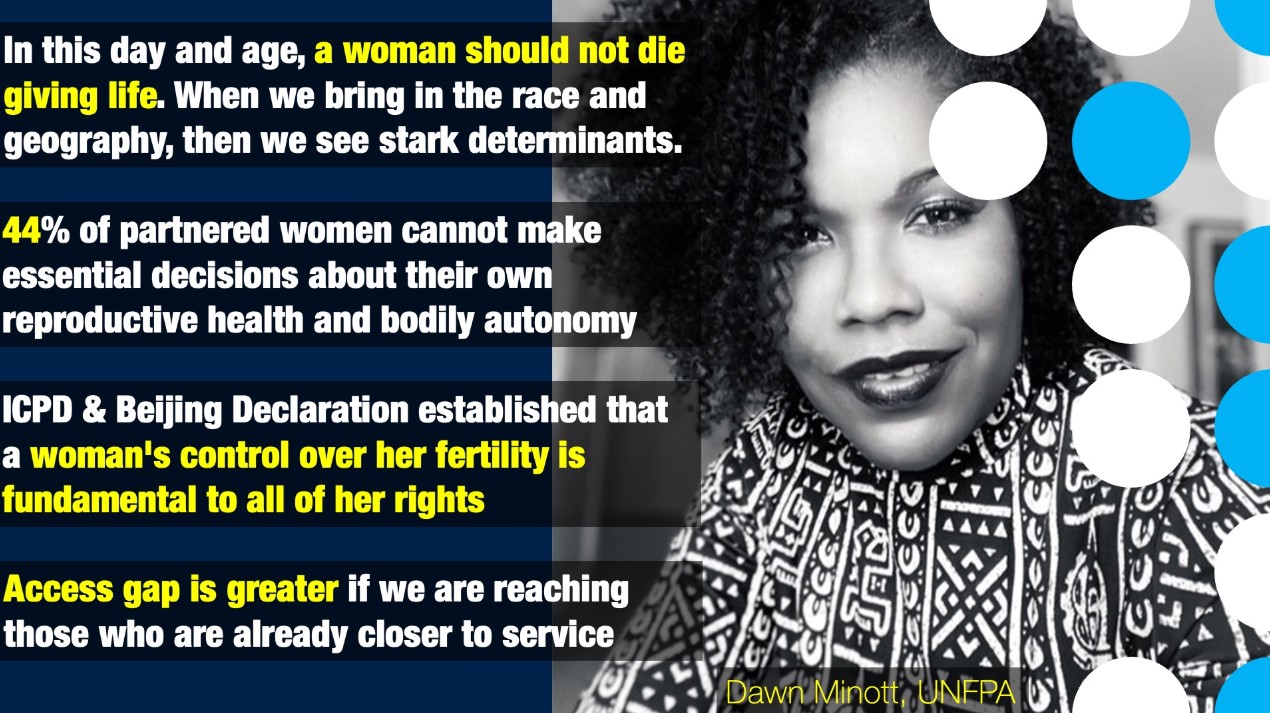
The WHO’s message highlights the importance of consulting qualified healthcare professionals before taking antibiotics. A doctor can determine whether your illness is bacterial or viral and prescribe treatment accordingly. Self-medicating with antibiotics can lead to unnecessary complications and exacerbate the issue of resistance.
The rise of antibiotic resistance is a pressing global health challenge. Addressing this crisis requires collective action from governments, healthcare providers, and the public. Here are some key measures:
1. Education and Awareness: Public health campaigns should emphasize the appropriate use of antibiotics and the dangers of resistance.
2. Stricter Regulations: Governments must enforce policies to prevent the over-the-counter sale of antibiotics without a prescription.
3. Investment in Research: Pharmaceutical companies and research institutions should prioritize the development of new antibiotics and alternative treatments.
4. Global Cooperation: Countries must collaborate to track and address resistance patterns worldwide.
Doctors, nurses, and pharmacists play a crucial role in promoting responsible antibiotic use. By educating patients about the differences between bacterial and viral infections, healthcare providers can reduce unnecessary prescriptions.
Takeaway for Patients
• As patients, it’s our responsibility to use antibiotics wisely. Here’s how you can contribute:
• Ask Questions: If your doctor prescribes antibiotics, ask whether they’re necessary and what alternatives might exist.
• Follow Instructions: Take the full course of antibiotics as prescribed, even if you start feeling better before finishing.
• Avoid Self-Medication: Never take leftover antibiotics or use someone else’s prescription.
The misuse of antibiotics doesn’t just affect individuals, it has far-reaching consequences for society. Resistant infections strain healthcare systems, increase medical costs, and limit treatment options for future generations.
Antibiotics are life-saving drugs, but they are not the answer to every illness. Understanding when and how to use them is essential for protecting your health and combating antibiotic resistance. The next time you catch a cold or flu, remember that antibiotics won’t help. Instead, focus on supporting your immune system and seek guidance from a healthcare professional.
By using antibiotics responsibly, we can preserve their effectiveness for those who truly need them and contribute to a healthier, more resilient world

 The next time you catch a cold or flu, remember that antibiotics won’t help. Instead, focus on supporting your immune system and seek guidance from a healthcare professional.
The next time you catch a cold or flu, remember that antibiotics won’t help. Instead, focus on supporting your immune system and seek guidance from a healthcare professional.






.jpeg)




.jpeg)







.jpeg)



.jpeg)
.jpeg)