At 31, the California primary school chief was a perseverance competitor in remarkable condition. Despite the fact that he had asthma, Sipos had ascended Mount Whitney, the tallest mountain in the coterminous United States, finished an edge-to-edge climb in the Grand Canyon in a negligible 10 hours - at any rate two hours not exactly normal - and barely cared about timing 100-mile bicycle rides on ends of the week.
Be that as it may, in May 2001, his vitality was hailing. Sipos, who lived in Riverside, counseled his long-term general specialist, who requested blood tests that uncovered an unusually low iron level.
Quite a while later when he created foot torment, Sipos saw a podiatrist who revealed to him he had osteoarthritis, commonly brought about by mileage on joints. A couple of years after the fact, an expert analyzed his agonizing wrists and lower legs as rheumatoid joint inflammation, a genuine immune system malady. That was trailed by the analysis of an uncommon blood condition that a hematologist observed, yet didn't treat.
It wasn't until 2018 - almost 17 years to the day after he originally observed a specialist for weariness - that Sipos learned he had none of those diseases.
The news was conveyed by a pro whose delicate, estimated tone gave a false representation of the stunning message that electrifies Sipos: Without treatment, which was long past due, he could kick the bucket.
"We both began crying," Sipos reviewed of his response and that of his better half, Tami. "It felt like the oxygen had been drained out of the room."
He attributes his endurance to the ability and empathy of that expert, who keeps on administering his treatment.
Sipos confided in the family doctor, who had conveyed his children. The specialist disclosed to Sipos his weakness was the aftereffect of paleness and could be effectively rewarded with an over-the-counter iron enhancement that he should take when he felt uncommonly drained.
The pills appeared to work. "For the following 10 years I would pop iron pills now and then and notice a knock" in vitality, Sipos said.
In 2007 another issue emerged: The bottoms of his feet throbbed and consumed. He counseled a podiatrist who disclosed to Sipos he had "fallen curves" - level feet that create in adulthood. The specialist recommended orthotics. For some time, they subdued the agony.
By 2015, the foot torment was impressively more awful and had inundated his lower legs, stopping his support in extraordinary games. Sipos' hands felt shivery and numb and he alluded to a nervous system specialist and a rheumatologist.
The nervous system specialist revealed to Sipos he was experiencing carpal passage disorder - deadness or shivering in the hands brought about by a compacted nerve - just as fringe neuropathy, harm to the nerves outside the cerebrum and spinal rope.
"He said I ought to have it taken a gander at in light of the fact that somebody 46 years of age ought not to have neuropathy," Sipos was told. Fringe neuropathy can be brought about by an assortment of sicknesses, among them diabetes, liver ailment, and bone marrow issue.
The rheumatologist requested blood tests and analyzed "seronegative" rheumatoid joint inflammation. In spite of the fact that testing didn't demonstrate antibodies to the illness, his joint torment, the specialist stated, emphatically proposed it.
The rheumatologist endorsed two medications: methotrexate, chemotherapy sedate used to treat rheumatoid joint pain, and when that didn't help, hydroxychloroquine, an enemy of intestinal sickness tranquilize used to treat immune system issue. Neither worked.
By then, Sipos reviewed, the agony was so serious "the heaviness of the [bed] sheets would feel like my feet were being squashed." He wore supports on his wrists and lower legs in a for the most part bombed endeavor to stifle the torment, and took the narcotic torment executioner hydrocodone to endure the day.
In 2016, Sipos counseled a subsequent rheumatologist. She concurred it was odd that neither one of the drugs had been viable and recommended different meds. At the point when they fizzled, she requested a test for immunoglobulin M (IgM) antibodies, which can evaluate invulnerable capacity. The test demonstrated an "m spike," a sign that Sipos may have a precancerous condition or potentially numerous myeloma, a phenomenal malignant growth.
In mid-2017 she alluded Sipos, who by then was experiencing successive night sweats, to a pro who treats blood issues.
The hematologist quickly requested pee and blood tests. Based on those, Sipos stated, she guaranteed him he didn't have malignant growth, yet rather a precancerous condition called MGUS, short for monoclonal gammopathy of unsure importance.
MGUS is regularly found by chance when specialists are searching for different things. It regularly causes no side effects yet should be observed intently on the grounds that in about 1% of patients every year it can advance to numerous myeloma, a disease of plasma cells, or another harm. In the event that there is no movement, treatment is normally not required.
"She said the standard of care was watch and pause," Sipos reviewed. That implied arrangements like clockwork to check his blood and pee.
Sipos said the specialist likewise played out a few bone marrow biopsies yet the outcomes were uncertain.
At the point when he got some information about the unwavering consuming agony in his grasp and feet, she offered no clarification.
In mid-2018, he stated, he faced her. "I'm deteriorating," he said. Her answer was distinct. "She stated, 'Truly, you might be in a wheelchair, yet we could never treat this.' " His IgM level, she let him know, was not adequately raised to warrant the dangers of treatment, which would include chemotherapy. Attentive holding up was the most secure course.
The hematologist disclosed to Sipos he was allowed to look for a subsequent assessment. He was at first reluctant. Despite the fact that she was routinely an hour or two late for planned arrangements, the specialist "appeared to be so proficient and shrewd and would talk with such position," he said. In any case, at his significant other's encouraging, Sipos concluded it was the ideal opportunity for another master to say something.
What he didn't know was that hearing the second point of view would potentially spare his life.
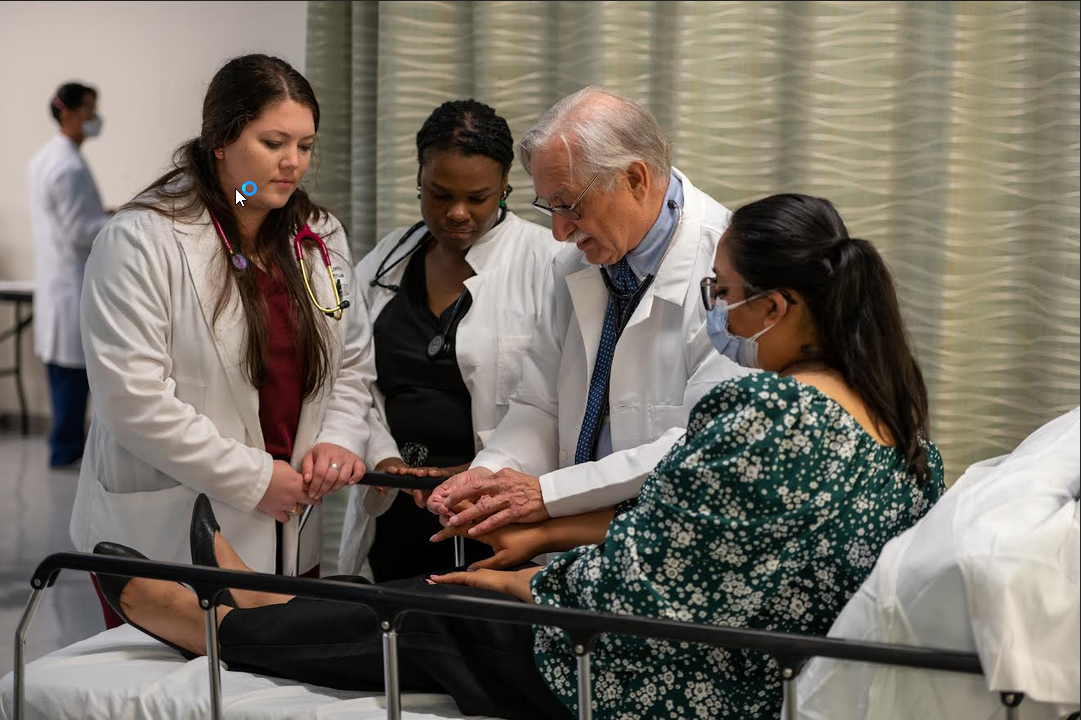
Sipos and his better half hung tight a month and a half for the interview with Muhammad Omair Kamal, an associate teacher of clinical oncology at Loma Linda University Cancer Center.
Moving his records to Kamal in anticipation of the arrangement was a battle, Sipos stated, requiring different calls by him just as Kamal's staff.
Both Jeff and Tami Sipos state that subtleties of the May 14, 2018, meeting are burned into their recollections.
"I recollect Dr. Kamal inclined forward and in his delicate, sweet voice brimming with concern stated, 'Mr. Sipos, has anybody disclosed to you have malignancy? Why you're not getting rewarded for this?' " Sipos reviewed.
The shocked couple rehashed what the hematologist had been stating for over a year: that Sipos didn't have malignancy and that observing was the best strategy.
Kamal arduously opposes this idea. "You have the disease," Sipos recalls that him saying. "On the off chance that you were my patient, you'd be begun on chemotherapy tomorrow." Then he gave the couple treatment rules from the National Cancer Institute.
In spite of the fact that he despite everything didn't have the entirety of Sipos' records, Kamal said he firmly speculated the chief had an uncommon, slow-developing type of B cell lymphoma called Waldenstrom macroglobulinemia, otherwise called Waldenstrom's or lymphoplasmacytic lymphoma. Kamal had seen four different cases in his vocation. MGUS can be an antecedent of numerous myeloma or Waldenstrom's. Sipos later discovered that a January 2017 pathology report referenced it as a potential reason for his side effects.
Around 1,500 cases are analyzed every year in the United States, contrasted with around 32,000 instances of different myeloma.
Waldenstrom's happens for the most part in men more than 60 when lymphoma cells in bone marrow multiply, swarming out ordinary red and white platelets. Sickliness is normal and indications incorporate exhaustion, neuropathy, and night sweats. There is no fix. Treatment ordinarily comprises of chemotherapy and focused on medicines that execute just malignant growth cells. The sickness is analyzed through blood tests and a bone marrow biopsy and can be affirmed by a test for a hereditary transformation.
Kamal said he can't comprehend why Sipos went undiscovered for such a long time. "He was seeing the correct specialist," Kamal noted, alluding to the best possible strength.
At the point when he got Sipos' finished records, Kamal stated, "lab after lab after lab" indicated results that justified treatment. "There are relatively few ailments [other than Waldenstrom's] where you see high IgM and neuropathy. Most patients are analyzed inside a year or two."
Sipos said that when he mentioned to the principal hematologist what Kamal had suggested, she shied away and demanded that her conclusion was right. Exchanging specialists were tricky; Kamal was outside his protection organization.
So one more month passed while Sipos, uncertain about what to do, got another feeling. The third malignant growth authority firmly favored Kamal. "On the off chance that you don't have chemo, you will terminate," Sipos recalls her platitude.
Sipos called his insurance agency and mentioned an exchange to Kamal; it was immediately affirmed.
He at that point experienced another bone marrow biopsy and testing to preclude amyloidosis, an uncommon illness brought about by the gathering of a protein that can bring about organ disappointment. A positive test for the MYD88 L265P change connected to Waldenstrom's secured the analysis. (The change isn't given to posterity.)
In mid-August 2018, Sipos started a tiresome chemotherapy routine to treat Waldenstrom's. He wore a Superman T-shirt that one of his kindergarten understudies had offered him to each meeting as such a charm. By January 2019, his malignant growth was going away.
In any case, the horrifying nerve harm to his hands and feet keeps on plaguing him. Kamal said the harm is most likely irreversible and may have happened in light of the fact that his malignancy went untreated for such a long time.
Sipos, who sees a torment pro, said he has been endorsed methadone, which "removes the punch from it."
He said he has learned through unpleasant experiences to pose inquiries.
"No solid grown-up male ought to be iron deficient," he said. "I wish I'd had the foresight
 Sipos, who lived in Riverside, consulted his longtime general practitioner, who ordered blood tests that revealed an abnormally low iron level.
Sipos, who lived in Riverside, consulted his longtime general practitioner, who ordered blood tests that revealed an abnormally low iron level.




.jpeg)

.jpeg)



.jpeg)







.jpeg)



.jpeg)