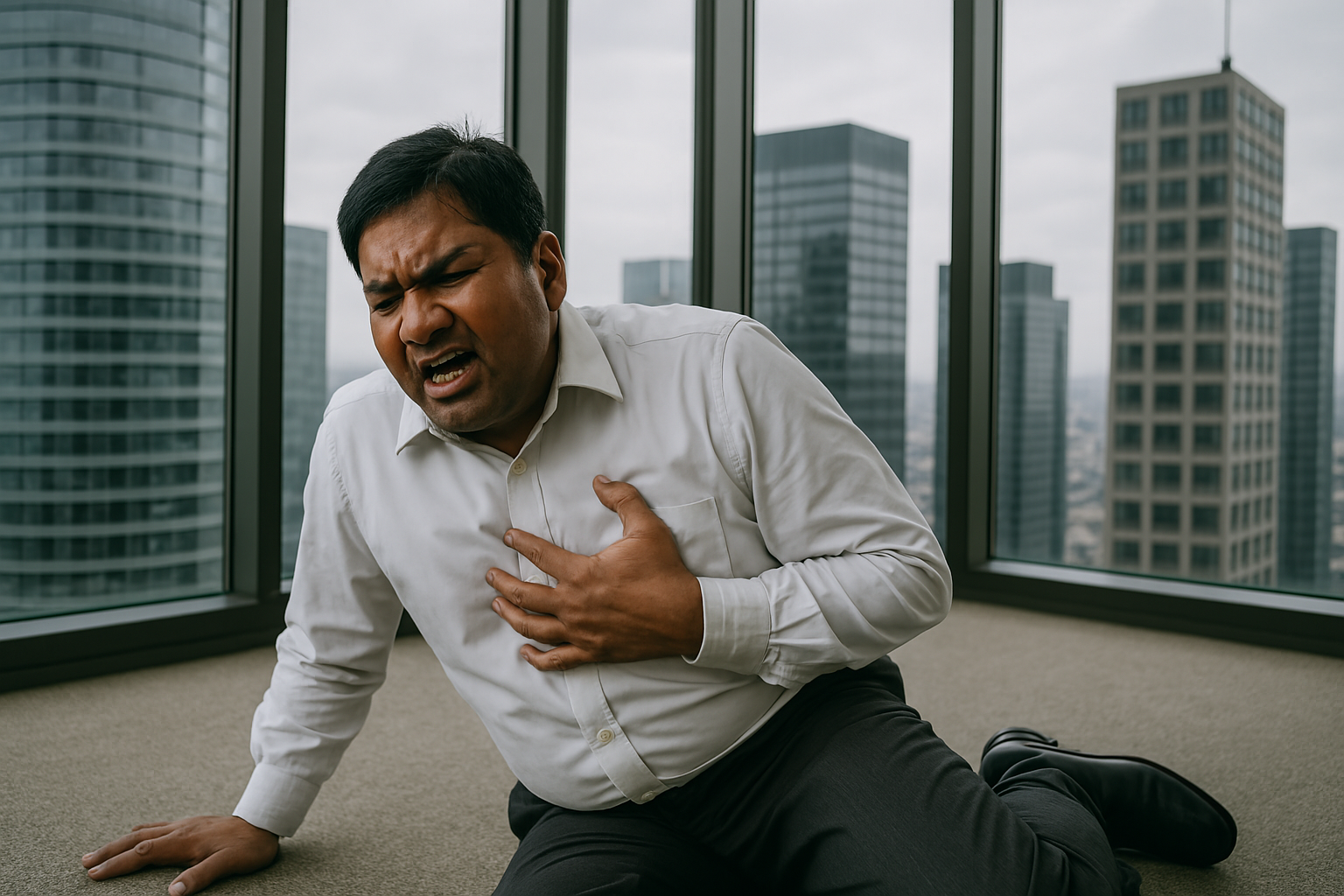
Pregnancy complications such as miscarriage, pre-eclampsia, diabetes in pregnancy (gestational diabetes) and pre-term birth are linked to a heightened risk of heart disease in later life, suggests an overarching (umbrella) analysis of data published by The BMJ recently.
Several other factors related to fertility and pregnancy also seem to be associated with subsequent cardiovascular disease, say the researchers, including starting periods early, use of combined oral contraceptives, polycystic ovary syndrome, and early menopause.
However, a longer length of breastfeeding was associated with a reduced risk of cardiovascular disease.
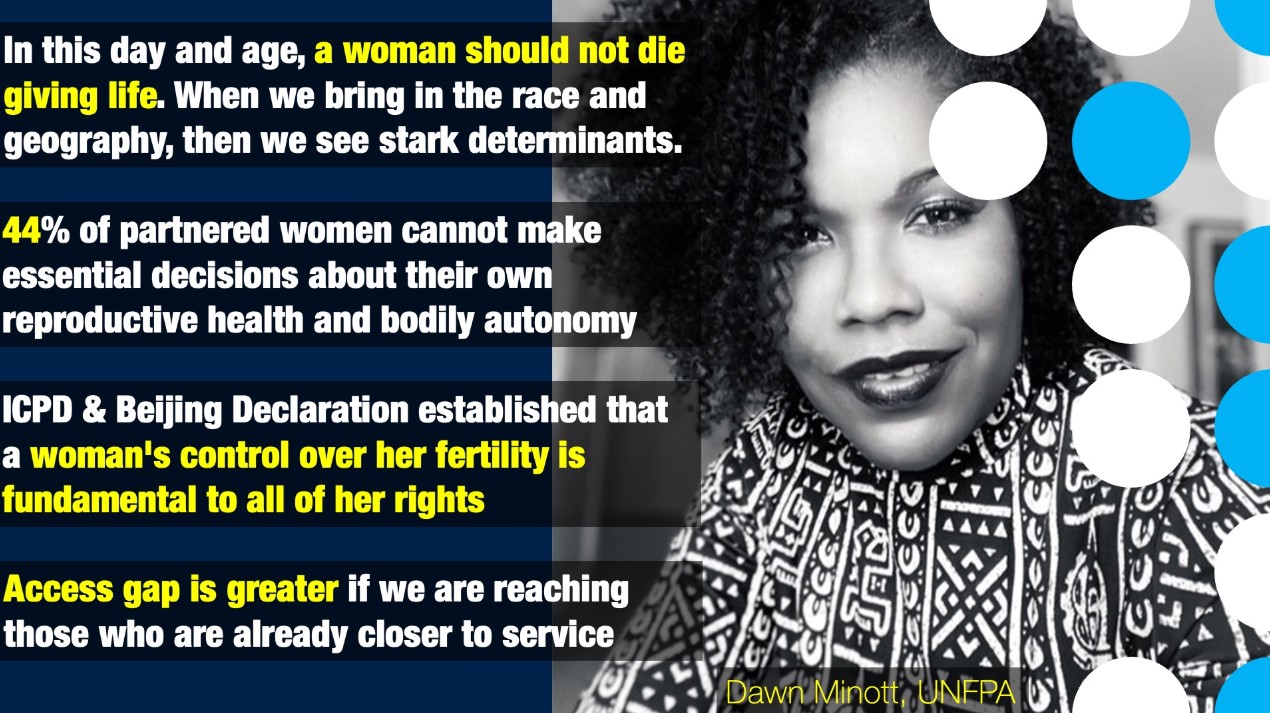
Previous research has suggested that risk factors specific to women may be linked to cardiovascular disease and stroke, but clarity on the quality of the evidence is lacking and on how the findings can be translated into public health and clinical practice.
So a team of UK researchers searched relevant research databases for published systematic reviews and meta-analyses that investigated links between reproductive factors in women of reproductive age and their subsequent risk of cardiovascular disease.
A total of 32 reviews were included, evaluating multiple risk factors over an average follow-up period of 7-10 years.
The researchers found that several factors, including starting periods early (early menarche), use of combined oral contraceptives, polycystic ovary syndrome, miscarriage, stillbirth, pre-eclampsia, diabetes during pregnancy, pre-term birth, low birth weight, and early menopause were associated with an up to twofold risk of cardiovascular outcomes.
Pre-eclampsia was associated with a fourfold risk of heart failure.
Possible explanations for these associations include family medical history, genetics, weight, high blood pressure and cholesterol levels, and chemical imbalances from use of hormonal contraceptives.
However, no association was found between cardiovascular disease outcomes and current use of progesterone only contraceptives, use of non-oral hormonal contraceptive agents, or fertility treatment.
What’s more, breastfeeding was associated with a lower risk of cardiovascular disease.
The researchers point to some limitations, such as missing data and the fact that reviews were largely based on observational evidence, so they cannot rule out the possibility that other unmeasured (confounding) factors may have had an effect.
Nevertheless, they say the evidence reported in this umbrella review suggests that, from menarche to menopause, the reproductive profile of women is associated with their future risk of cardiovascular disease.
It also provides clarity on the quality of the evidence, identifies gaps in evidence and practice, and provides recommendations that could be incorporated into guidelines, such as incorporating reproductive risk factors as part of the risk assessment for cardiovascular disease, they conclude.

 Along with several other factors, including starting periods early, use of combined oral contraceptives, and early menopause
Along with several other factors, including starting periods early, use of combined oral contraceptives, and early menopause







.jpeg)




.jpeg)






.jpeg)



.jpeg)
.jpeg)