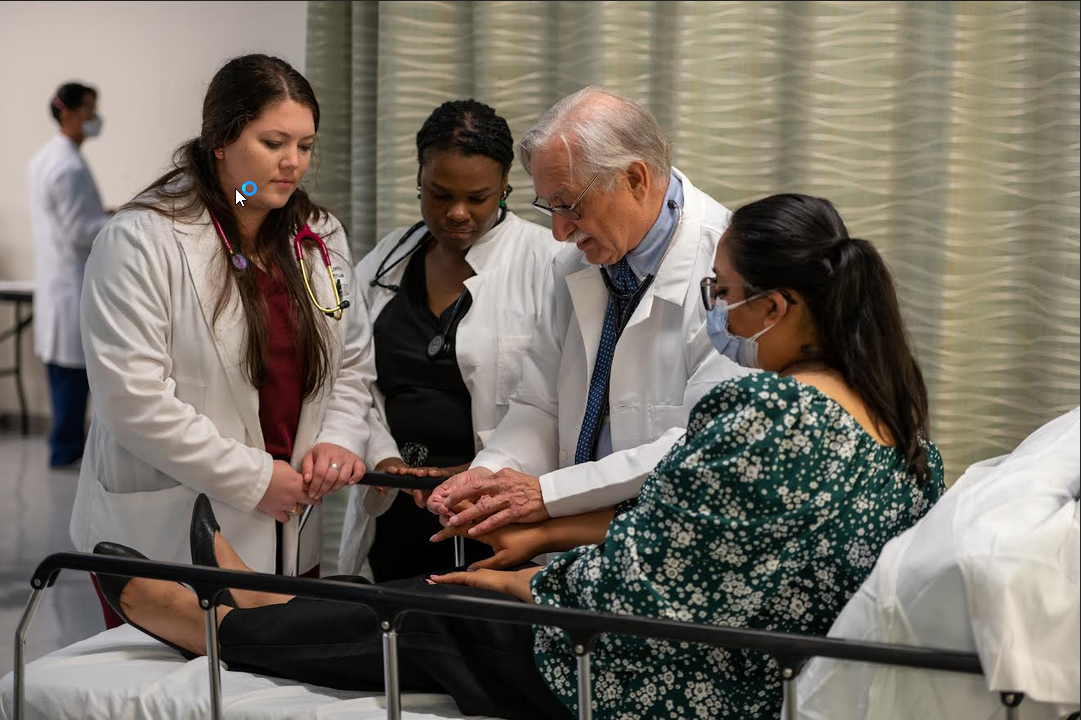
A trial published by The BMJ recently shows that regular breast examination by trained female health workers in Mumbai led to earlier diagnosis and reduced deaths from breast cancer in women aged 50 and older.
The researchers say this type of examination (known as clinical breast examination or CBE) should be considered as an alternative to x-ray (mammography) screening in low and middle-income countries.
Breast cancer rates are rising across the world, but particularly so in low and middle-income countries.
Mammography is the established screening tool in developed countries, but its cost and complexity mean it might not be an appropriate approach in low and middle-income countries. What’s more, most women in low and middle-income countries are younger than 50, and mammography is less effective in this age group.
Although clinical breast examination is an alternative screening method, doctors are still not sure if it can reduce deaths from breast cancer.
So a research team based in Mumbai set out to test if screening by clinical breast examination could result in earlier diagnosis and reduced mortality from breast cancer when compared with no screening.
Their findings are based on 20 years of data from 151,538 women aged 35-64 with no history of breast cancer who were living in 20 geographically distinct clusters in Mumbai, India.
Women were randomly allocated to 10 screening and 10 control arms.
Women in the screening arm (75,360) received four screening rounds of clinical breast examination (conducted by trained female primary health workers) and cancer awareness every two years, followed by five rounds of active surveillance every two years.
Women in the control arm (76,178) received one round of cancer awareness followed by eight rounds of active surveillance every two years.
Breast cancer was detected at an earlier age in the screening arm than in the control arm (55 v 57 years), with a significant reduction in the proportion of women with more advanced (stage III or IV) disease (37% v 47%) - known as downstaging.
Across all ages, clinical breast examination led to a non-significant reduction in breast cancer mortality in the screening arm versus the control arm (21 v 25 deaths per 100,000 person-years).
However, a significant reduction in breast cancer mortality of nearly 30% was seen in women aged 50 and older (25 v 35 deaths per 100,000 person-years). In women younger than 50, despite successful downstaging, no mortality reduction was seen. There was a 5% reduction in all-cause mortality in the screening arm compared with the control arm, but it was not statistically significant.
The researchers point out that some cancer staging data and cause of death information may have been missed, and that some residual uncertainty cannot be excluded.
However, this was a well-designed trial carried out by researchers with a full understanding of the realities that influence the conduct of complex, public health randomised trials in low and middle-income countries.
As such, they say: “Our study suggests that implementation of population screening by clinical breast examination in low and middle-income countries is feasible, provided that adequate training of screening providers, careful monitoring, and quality of performance are assured.”
And they conclude: “Clinical breast examination should be considered for breast cancer screening in low and middle-income countries.”

 Regular clinical breast examination should be considered in low and middle-income countries, say, researchers
Regular clinical breast examination should be considered in low and middle-income countries, say, researchers






.jpeg)

.jpeg)



.jpeg)







.jpeg)



.jpeg)