Breakthroughs in science often redefine the way we approach healthcare, and an innovation by bioengineers is poised to do just that. Researchers at Rice University have created a “construction kit” to build custom sense-and-respond circuits in human cells. This revolutionary technology has the potential to transform therapies for complex diseases such as cancer and autoimmune disorders, providing a glimpse into the future of personalized medicine.
Imagine a world where cells in your body act like tiny computers, processing signals and responding to threats with precision. That’s the essence of what these new circuits promise. These circuits are designed to identify specific signals such as markers of inflammation or tumor growth and trigger precise, preprogrammed responses.
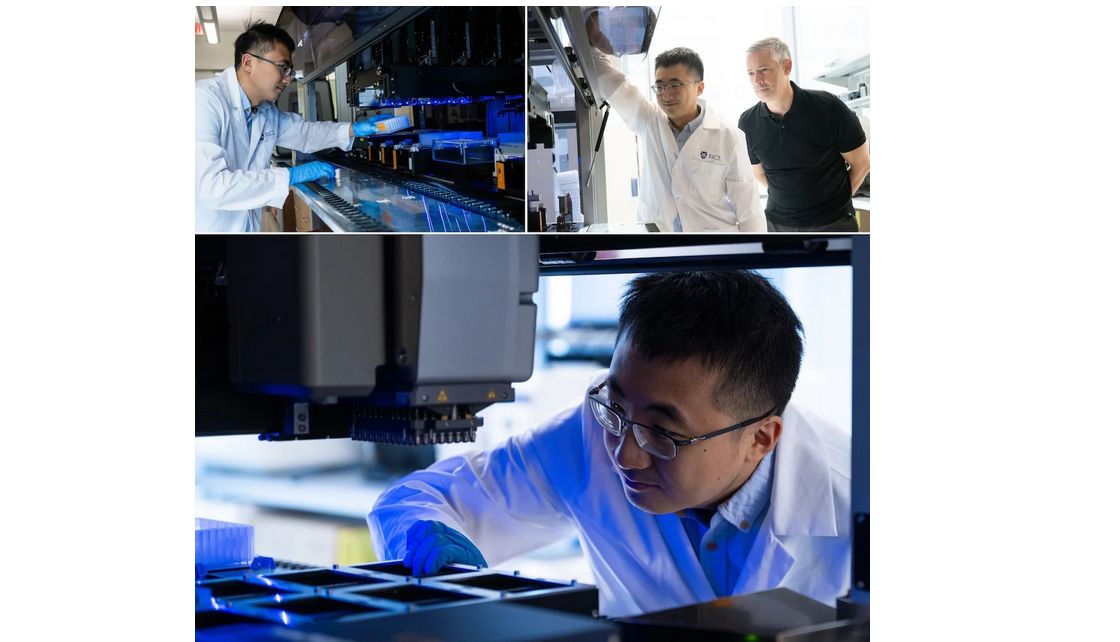
Xiaoyu Yang, a graduate student at Rice University and the lead author of this study published in Science, explains, “This work brings us closer to building ‘smart cells’ capable of detecting disease and releasing treatments immediately.”
This innovation is a leap forward in the field of synthetic biology, which focuses on reprogramming living cells to perform specific tasks. The construction kit developed by the researchers relies on a natural cellular process called phosphorylation, a critical function cells use to respond to environmental changes.
What Is Phosphorylation?
Phosphorylation is a natural mechanism where a phosphate group is added to a protein, activating or deactivating it to initiate specific functions. This process plays a crucial role in cellular responses, from fighting pathogens to gene expression. It’s like a cascade of falling dominoes: one small change triggers a chain reaction leading to a significant outcome.
Previously, scientists attempted to harness phosphorylation for therapeutic purposes by re-engineering the body’s existing pathways. However, the sheer complexity of these systems made them difficult to manipulate effectively. Rice University’s research has overcome this barrier by providing a simpler, modular approach to building new pathways from scratch.
How Smart Cells Work
The circuits built using this new kit essentially function as decision-makers within the cell. They “sense” specific biochemical signals, such as high blood sugar levels or markers of inflammation, and “respond” with a tailored action. For example, a cell could detect the presence of a cancer marker and release a therapeutic protein to neutralize it, all without external intervention.
This approach is revolutionary for several reasons:
Precision: Unlike traditional therapies, which can have widespread effects, these circuits allow for highly targeted treatments.
Customizability: The circuits can be designed to address specific diseases or conditions based on an individual’s needs.
Efficiency: By programming cells to respond instantly, treatments can be delivered exactly when and where they are needed.
The potential applications of this technology are vast. Here are a few areas where it could have the most significant impact:
1. Cancer Treatment
Cancer therapies often struggle with targeting only cancerous cells while leaving healthy cells unharmed. With smart cells, therapies could be programmed to activate only in the presence of specific tumor markers, reducing side effects and increasing effectiveness.
2. Autoimmune Diseases
Autoimmune diseases occur when the immune system mistakenly attacks healthy tissues. Smart cells could detect the inflammatory signals that trigger these attacks and release molecules to suppress the immune response, providing relief without the need for broad-spectrum immunosuppressants.
3. Diabetes Management
For people with diabetes, blood sugar levels can fluctuate unpredictably. Smart cells could monitor glucose levels in real time and release insulin or other hormones as needed, potentially eliminating the need for constant blood sugar monitoring and injections.
4. Infectious Diseases
Infections often require immediate and targeted responses. Smart cells could be designed to recognize specific pathogens and produce antimicrobial peptides or other therapeutic agents to neutralize the threat.
The idea of engineering cells to respond to disease is not new, but previous attempts were limited by the complexity of natural signaling pathways. These pathways often involve multiple steps and are challenging to reconfigure without disrupting normal cellular functions.
The Rice University team’s innovation bypasses these challenges by introducing entirely new circuits that integrate seamlessly with the cell’s existing machinery. This modular approach simplifies the process and expands the range of potential applications.
While the potential of this technology is enormous, several challenges remain. For one, the safety of these engineered cells must be thoroughly tested to ensure they do not cause unintended side effects. Additionally, scaling up the production of these circuits for widespread clinical use will require significant investment and research.
Despite these hurdles, the possibilities are exciting. In the coming years, we could see the development of therapies that not only treat but also prevent diseases by programming cells to act as sentinels, constantly monitoring and responding to threats.
This breakthrough represents more than just a technological advancement; it’s a paradigm shift in how we approach disease management. Traditional treatments often involve administering external agents, such as drugs or surgeries, to address a problem. In contrast, this new approach focuses on empowering the body to heal itself by reprogramming its basic building blocks—cells.
The impact of this technology could be particularly profound in developing countries, where access to healthcare is often limited. Smart cells could provide a cost-effective, long-term solution to managing chronic conditions and diseases, reducing the burden on healthcare systems and improving the quality of life for millions.
The development of custom sense-and-respond circuits in human cells is an achievement in synthetic biology. By harnessing the natural process of phosphorylation, scientists at Rice University have created a tool that could revolutionize therapies for complex diseases like cancer and autoimmune disorders.
As research continues, the dream of “smart cells” that detect and treat disease autonomously is becoming a reality. This innovation holds the promise of a future where medicine is not just reactive but proactive, where treatments are not only effective but also tailored to individual needs.
In this new era of cellular engineering, the possibilities are as vast as they are exciting. The question is not if this technology will change healthcare but when, and the answer may be sooner than we think
 This innovation holds the promise of a future where medicine is not just reactive but proactive, where treatments are not only effective but also tailored to individual needs.
This innovation holds the promise of a future where medicine is not just reactive but proactive, where treatments are not only effective but also tailored to individual needs.











.jpeg)

.jpeg)
.jpeg)

.jpeg)


.jpeg)



.jpeg)
.jpeg)
.jpeg)


.jpg)


.jpeg)
.jpeg)