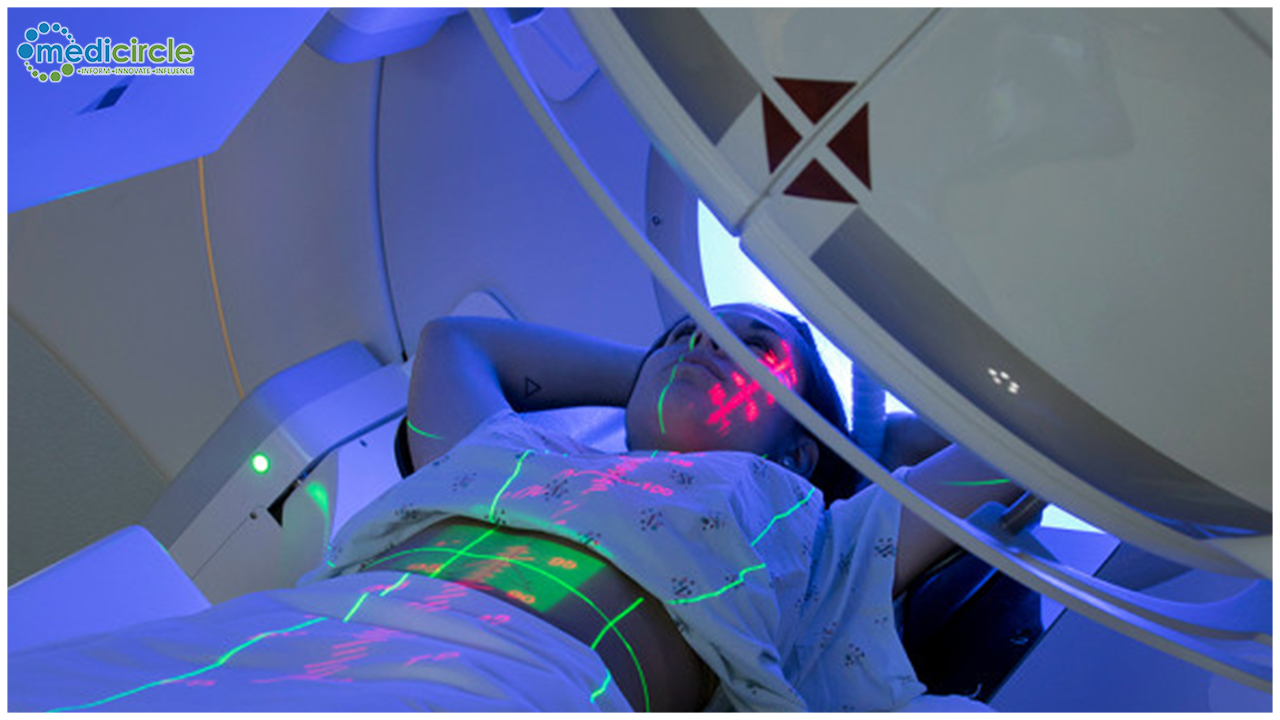
According to an IANS report, supercharging the mutation rate in cancer cells can create a powerful vaccine that is able to boost the effectiveness of immunotherapy, says a major new study. Scientists forced cancer cells in the lab to evolve much more rapidly than usual using a molecule called APOBEC3B, which is often used by tumours to drive rapid genetic change and drug resistance.
These highly mutated cancer cells could be used to create a vaccine for each individual cancer type, which amplified the effects of immunotherapy - and cured mice with a variety of otherwise treatment-resistant tumours showed the study published in the journal Nature Communications.
"Our new study rather paradoxically takes advantage of a mechanism used by cancers to rapidly evolve and become resistant to chemotherapy, and instead makes them much more vulnerable to the effects of immunotherapy," said study author Alan Melcher, Professor of Translational Immunotherapy at The Institute of Cancer Research, London.
"We have supercharged genetic changes in cancer in order to create cancer vaccines, which are tailored to the genetic code of these tumours, and can boost the immune response against them," Melcher said.
The researchers first showed they could drive rapid genetic changes in human cancer cells in the lab using high levels of APOBEC3B, which is able to edit the DNA code of cells, giving rise to genetic changes that can be seen as 'signatures' or 'footprints'.
The genetic analysis revealed more than a million extra mutations in the cells expressing APOBEC3B, compared with control cells.Of these, around 68,000 contained the classical APOBEC signature. These genetic signatures made cancer cells vulnerable to treatment with immune checkpoint blockade, a major strategy in immunotherapy.
However, by generating new genetic changes, APOBEC3B can also drive cancer evolution and help cancer cells become resistant to chemotherapy.So rather than give APOBEC3B directly to tumours as a treatment, the researchers instead used the genetic signature it left behind to create individual cancer vaccines, each tailored to the particular genetic profile of a specific.
STORY SOURCE:IANS
 The researchers first showed they could drive rapid genetic changes in human cancer cells in the lab using high levels of APOBEC3B, which is able to edit the DNA code of cells, giving rise to genetic changes that can be seen as 'signatures' or 'footprints'.
The researchers first showed they could drive rapid genetic changes in human cancer cells in the lab using high levels of APOBEC3B, which is able to edit the DNA code of cells, giving rise to genetic changes that can be seen as 'signatures' or 'footprints'.








.jpg)

.jpeg)

.jpg)





.jpeg)



.jpg)






.jpg)