In a recent study published in the Journal of the American College of Surgeons, a team of experts in bariatric and transplant surgery has shed light on the potential benefits of metabolic and bariatric surgery for individuals suffering from end-stage renal disease (ESRD) and obesity. Led by Dr. Anil Paramesh, the study aimed to explore whether such surgical interventions could improve the eligibility of ESRD patients for kidney transplantation, offering a glimmer of hope for those facing significant health challenges.
The prevalence of obesity all over the world has reached alarming levels, posing a significant barrier to transplant eligibility for many individuals. Recognizing the urgent need to address this issue, particularly among underserved populations, Dr. Paramesh and his team established the Collaborative for Obesity Research in Transplantation (CORT) initiative. This collaborative effort aimed to investigate potential solutions to improve outcomes for ESRD patients with obesity-related complications.
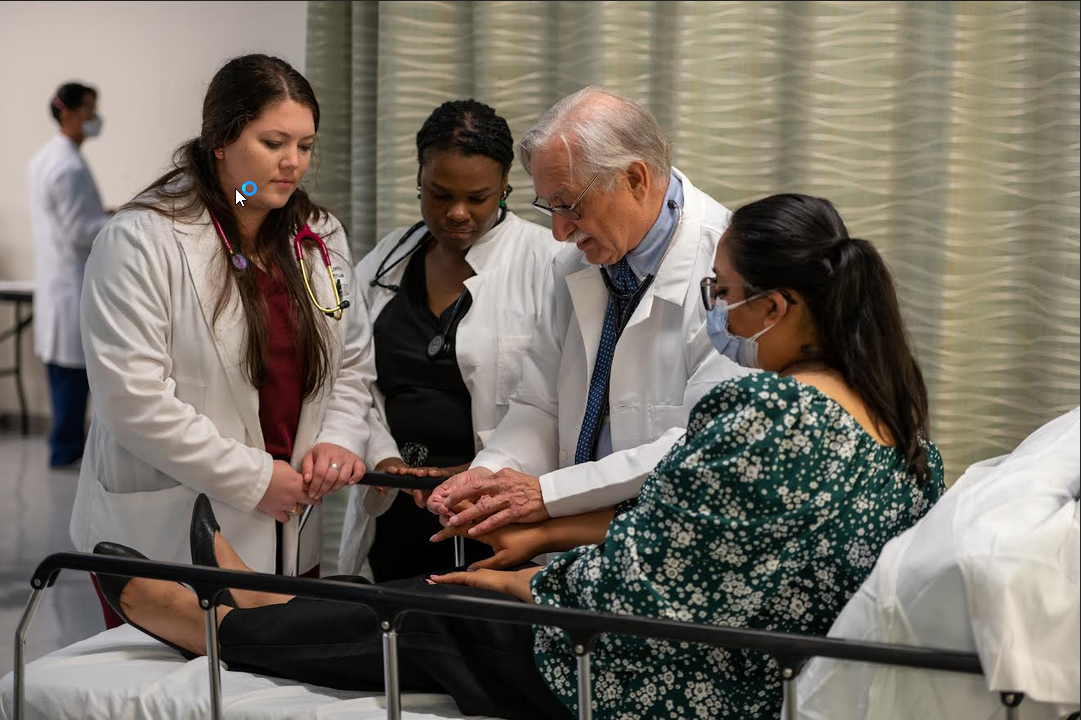
Dr. Paramesh, a distinguished professor of surgery, urology, and pediatrics, as well as the director of kidney and pancreas transplant programs at Tulane University School of Medicine, emphasized the profound impact of obesity on the lives of ESRD patients. Without access to kidney transplantation, these individuals are left with limited options, often resorting to costly and burdensome dialysis treatments that significantly diminish their quality of life.
The study, conducted over a period of four years from January 2019 to June 2023, enrolled 183 ESRD patients who were referred for bariatric surgery. Of these patients, 36 underwent weight loss surgery, with 10 subsequently receiving kidney transplants. The results were promising, revealing a 27% reduction in average body mass index (BMI) at the time of transplant, accompanied by improvements in the management of hypertension and diabetes.
He highlighted the significance of these findings, revealing the potential of bariatric surgery to address not only obesity but also other serious comorbid conditions such as diabetes, high blood pressure, and sleep apnea. By improving the overall health of patients and enhancing the viability of kidney transplants, this approach offers a ray of hope for individuals who were previously deemed ineligible for transplantation due to obesity-related concerns.
Despite the promising outcomes, the study encountered several challenges, including a high dropout rate among patients unwilling or unable to undergo surgery, as well as unique postoperative complications such as hypotension. Dr. Paramesh emphasized the need for enhanced patient education and support to ensure that potential candidates fully understand the benefits of weight loss surgery and its role in improving their eligibility for transplantation.
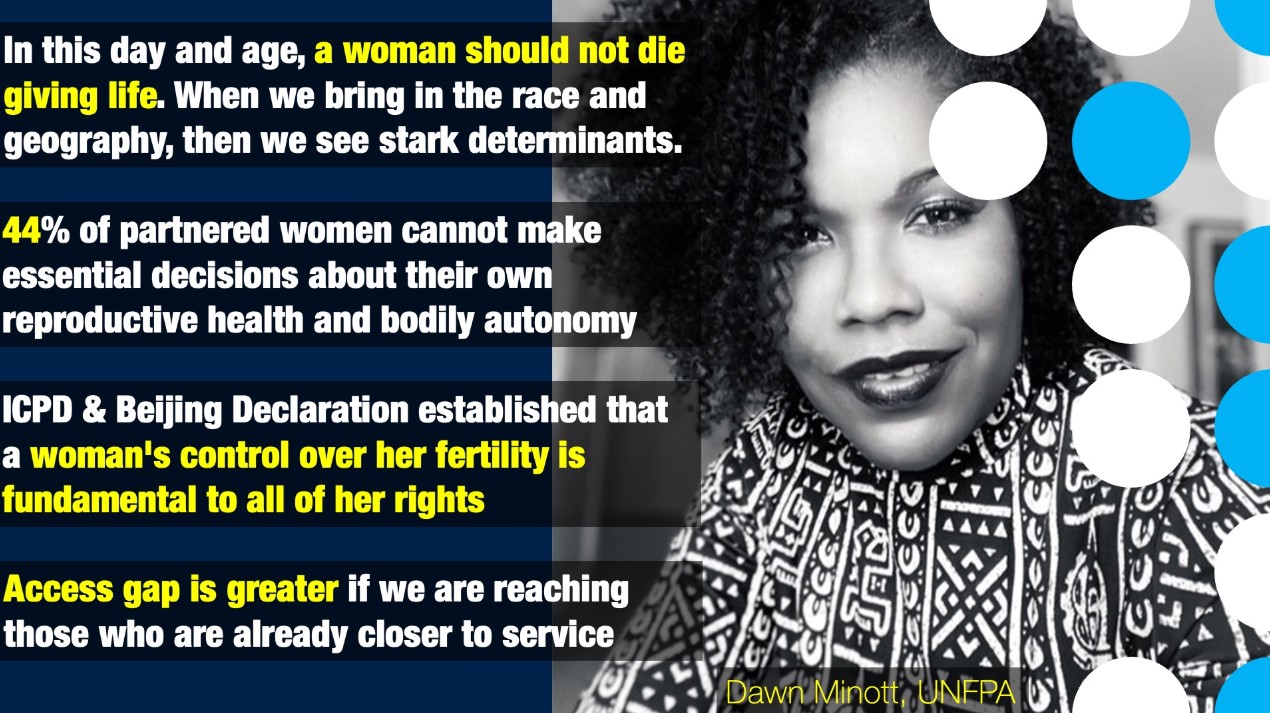
Moreover, Dr. Paramesh emphasized the broader implications of the study in addressing healthcare disparities, particularly among Black and lower-income individuals disproportionately affected by obesity-related diseases. By offering a comprehensive approach to healthcare that addresses both weight management and chronic disease management, bariatric surgery has the potential to narrow the gap in access to transplantation and improve outcomes for marginalized populations.
In conclusion, the collaborative efforts of bariatric and transplant surgery teams have yielded promising results in the quest to improve outcomes for ESRD patients with obesity. The study highlights the potential of metabolic and bariatric surgery to not only facilitate weight loss but also to enhance overall health and transplant eligibility. Moving forward, continued research and investment in patient education and support will be essential to maximize the benefits of these interventions and ensure equitable access to transplantation for all individuals in need.

 The study highlights the potential of metabolic and bariatric surgery to not only facilitate weight loss but also to enhance overall health and transplant eligibility.
The study highlights the potential of metabolic and bariatric surgery to not only facilitate weight loss but also to enhance overall health and transplant eligibility.



















.jpeg)


.jpeg)


.jpeg)
.jpeg)





.jpeg)





