If we are to end TB as promised by all the governments of African countries and globally, we need to find all people with TB, link them to effective standard treatment and care. If full cascade of TB services fails to reach people with TB, then not only will it result in avoidable human suffering but also fail us in stopping the spread of infection. Finding TB remains the critical entry-point to TB care pathway.
The sense of urgency is palpable with only 84 months are left to end TB by 2030. "In the African region we have an alarmingly high number of TB-HIV co-infections. One in three people with HIV is killed by TB. We will not be able to end AIDS unless we end TB. We have to bring TB services closer to the people and diagnose people with TB and HIV as early as possible. We need the TB services to come so close to the people that there will be no barriers between the people and the service, because as of now, we have a lot of barriers impeding people’s access to existing services," said Dr Lucica Ditiu, Executive Director of Stop TB Partnership at the 22nd International Conference on AIDS and STIs in Africa (22nd ICASA), in Harare, Zimbabwe.
Dr Ditiu is right: More than half of the people with TB in Africa do not even get a WHO recommended molecular test diagnosis. As per the latest Global TB Report of the World Health Organization (WHO) only about four out of ten people who got diagnosed with TB in the African region had received a WHO recommended molecular test diagnosis in 2022.
There are several reasons for this: one is the still used outdated 140 years old microscopy test, which has poor sensitivity and misses many TB cases; the other and more important one is the lack of access to the currently available WHO recommended highly sensitive molecular diagnostics, especially for populations in rural and hard to reach areas where the need is the greatest. That is why WHO’s highest level initiative launched in 2018 (Find.Treat.All) had called on governments to replace microscopy 100% with upfront molecular tests by 2027. This call to completely replace microscopy with molecular tests to diagnose TB was reechoed in September 2023 by world leaders who met at the UN High Level Meeting on TB. Yet, less than half of people with TB worldwide got a molecular test diagnosis as per the latest WHO report launched last month.
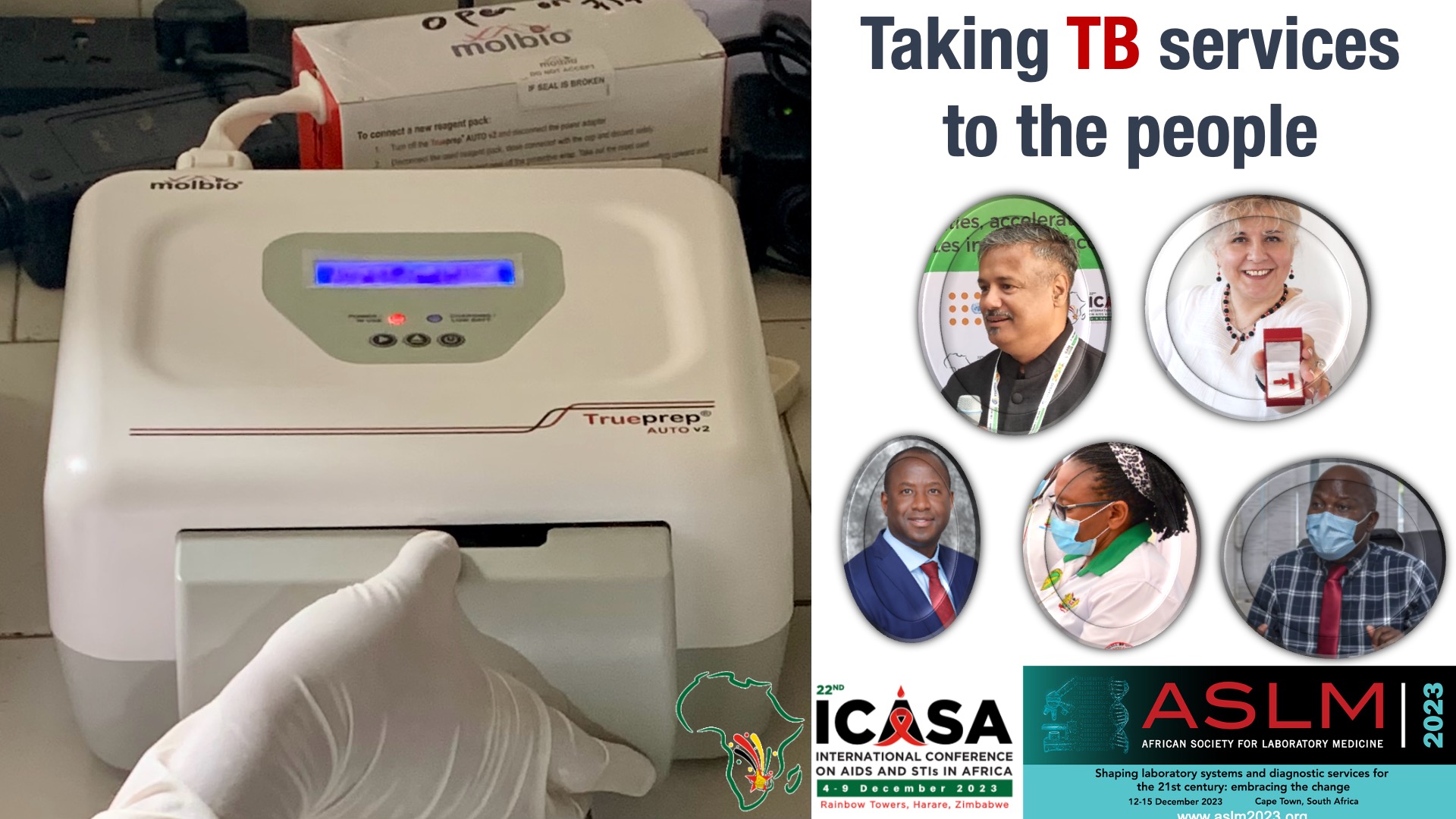
Sumit Mitra, the President of Global Sales and Marketing, Molbio Diagnostics (the makers of Truenat, which is the only WHO recommended point of care, decentralized, and laboratory independent molecular test globally), says it is only possible to have inclusive healthcare if a certain demographic is included. “We have to bring the laboratory to the people.” He says diagnostics have shifted from being laboratory-centric to people-centric. “That is how we will win the battle against TB,” said Mitra at the 6th biennial conference of African Society for Laboratory Medicine (ASLM) in Cape Town, South Africa.
Mitra’s call to bring TB services to the people reiterates the Global Call to Find All TB to Stop TB (www.bit.ly/findalltb) launched in Goa, India last month, and whose Africa launch took place last week at 22nd ICASA in Zimbabwe. Over 350 endorsements worldwide support this call to demand:
100% replacement of smear microscopy with WHO-recommended molecular tests as soon as possible, along with a paradigm shift from a lab-centric to a fundamentally people-centric model to find TB, leaving no one behind
Find the millions of people who are missed by the TB services! Screen everyone (and not just those with TB symptoms) with WHO-recommended screening tools and use molecular tests to confirm the disease in those with presumptive TB.
Truenat: This time for Africa
Speaking on the sidelines of the 6th biennial conference of African Society for Laboratory Medicine (ASLM) in Cape Town, South Africa, Mitra said that with the Truenat molecular test being piloted in over 18 African countries, the response so far has been good.
At first glance it does not look like much- just a small portable device with little or no paraphernalia that usually accompanies cutting-edge technology. Yet, Truenat has revolutionized TB diagnostics, as it plays the dual role of using the new molecular testing, and also bringing the laboratory to the doorsteps of communities.
Truenat is small enough to be set up on a small table; it is battery-operated, needs no electricity, and is built to operate in peripheral settings where power outages are common and air conditioning is scarce. For example, Stop TB Partnership documents how solar power is used to charge Truenat in Democratic Republic of Congo in remote settings. Truenat has the added function of a 35-minute wait time for results. “This is perfect.” The technicians and the clients do not wait hours for results, which is a big challenge for people in rural areas who have a certain amount of day light hours to work and cannot afford long waits.
Joseph Bitilinyu-Bangoh, Deputy Director in the office of the Ministry of Health in Malawi, said at ASLM that his country has four Truenat molecular test machines in use in remote areas. Those communities would never have been served as the roads are mostly inaccessible. “So far, our medical officers are happy with the testing, and we hope to get four more machines. It has been a real game changer for us.”
Catherine Githinji from the national TB programme of Kenya, says that with the help of United States Agency for International Development (USAID) and Stop TB Partnership, the country has placed 30 Truenat molecular test machines throughout the seven counties of Kenya. It will distribute another 48 machines through the Global Fund to Fight AIDS, Tuberculosis and Malaria (The Global Fund) in the coming year.
Githinji says the initial rollout of the machines was a little bumpy, as is expected with all innovations as it takes some time to learn how to manage the tools, but now the process is smooth. “We are seeing good results; there is a collaboration between the mobile machines and the static laboratories, increasing testing.”
Mitra adds that in the Philippines, medics took the Truenat in a small utility boat, hopping from one islet to another islet, testing communities. As a result, active case detection rate of TB went up by over 1200 percent. That is the kind of impact we want to make.”
He shared that beside TB, Truenat molecular test can diagnose over 40 diseases, such as Sexually Transmitted Infections (STIs), COVID-19, SARS, Malaria, Hepatitis, HPV, and Cholera, among others, and another 30 are in the pipeline.
An example of the versatility of Truenat is the recent experience in India, which bought 1700 machines in 2019 for the national TB programme, but before implementation, COVID-19 hit. The programme was re-purposed to deal with the COVID-19 pandemic. During the pandemic, India procured another 4000 Truenat machines: “that’s the beauty: you can create the diagnostic infrastructure organically,” said Mitra.
Earlier this year, the Stop TB Partnership, USAID, and the Global Fund stated that access to rapid molecular testing for TB is a human right. It also announced a substantial price cut to the Truenat TB diagnostic test under an agreement signed with Molbio Diagnostics. Under the agreement, the price of the Truenat MTB and MTB Plus test has come down to US$ 7.90 per test from the then price of US$ 9.
Additionally, Molbio Diagnostics has agreed to provide timely service and maintenance of their diagnostic instruments. This is particularly important for African governments, who often need help maintaining expensive lab equipment. This also resonates with the sentiments of ASLM Chief Executive Officer Nqobile Ndlovu, who says that manufacturers are increasingly asked to lease equipment and charge only for reagents to ease the cost of providing diagnostic equipment.
Zarina Geloo – CNS (Citizen News Service)
(Zarina Geloo is a freelance journalist based in Zambia writing on health and development, and part of CNS Correspondents Team. She is reporting from 6th biennial conference of African Society for Laboratory Medicine (ASLM) in Cape Town, South Africa)
 More alarming is the fact that in 2021, WHO estimated that 4.2 million people with TB were not even diagnosed, which is 40% of the overall estimated global burden of TB. This significant gap in access to standard diagnosis stands as one of the largest shortfalls in the global TB response.
More alarming is the fact that in 2021, WHO estimated that 4.2 million people with TB were not even diagnosed, which is 40% of the overall estimated global burden of TB. This significant gap in access to standard diagnosis stands as one of the largest shortfalls in the global TB response.










.jpeg)



.jpg)





.jpeg)

.jpg)




.png)

